Reacted to the message well
Medical Reimbursement
Feature for claiming all types of medical bills without any hassles
Timeline
2 Weeks
Users
3k+ in month 1
Revenue
60 Million+
Product manager
01
Designer
01
Developers
4
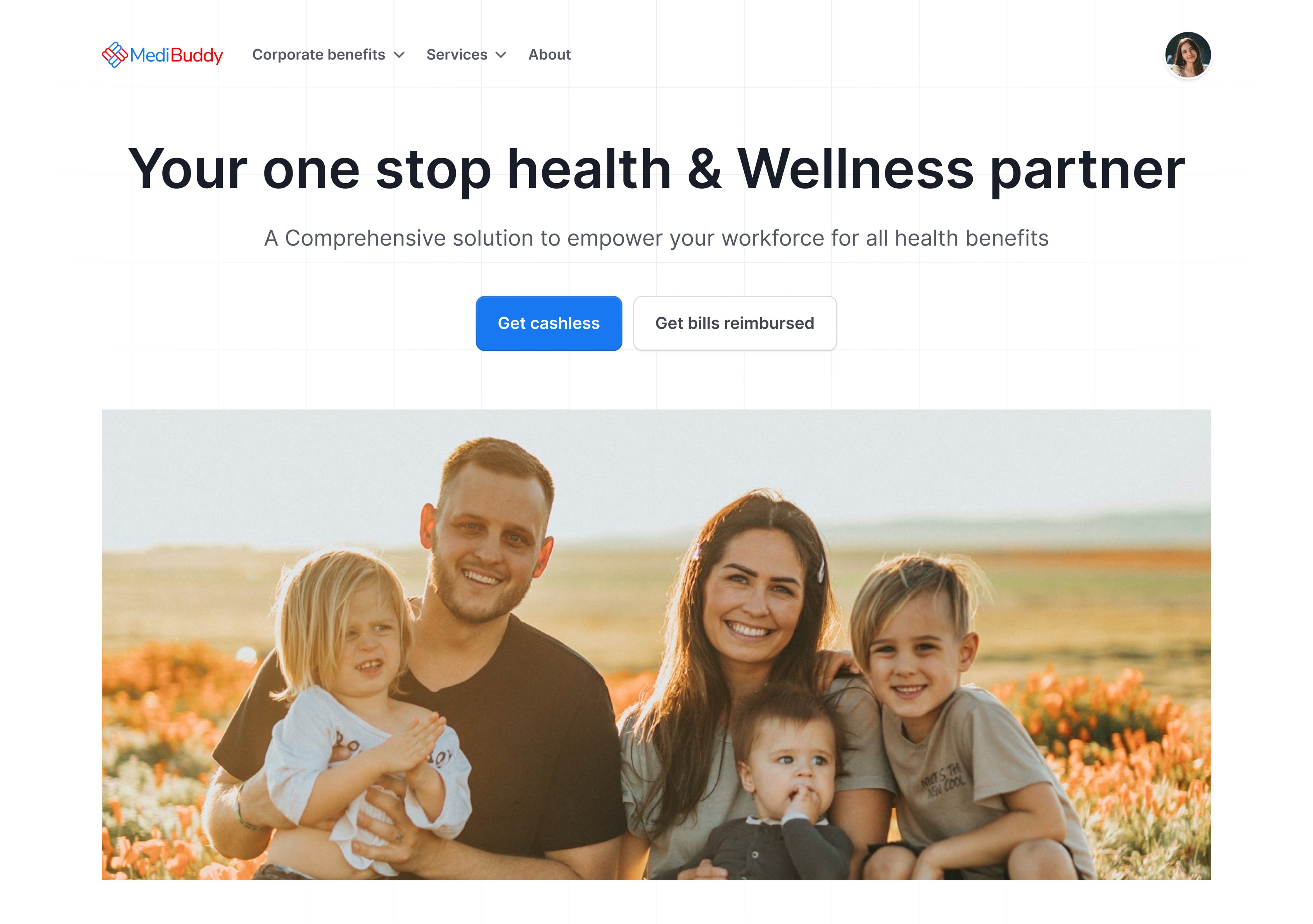
About
MediBuddy is India’s largest healthcare platform which provides online and offline healthcare services like online consultation, Lab test, Medicine delivery, Surgery care, Physiotherapy etc.
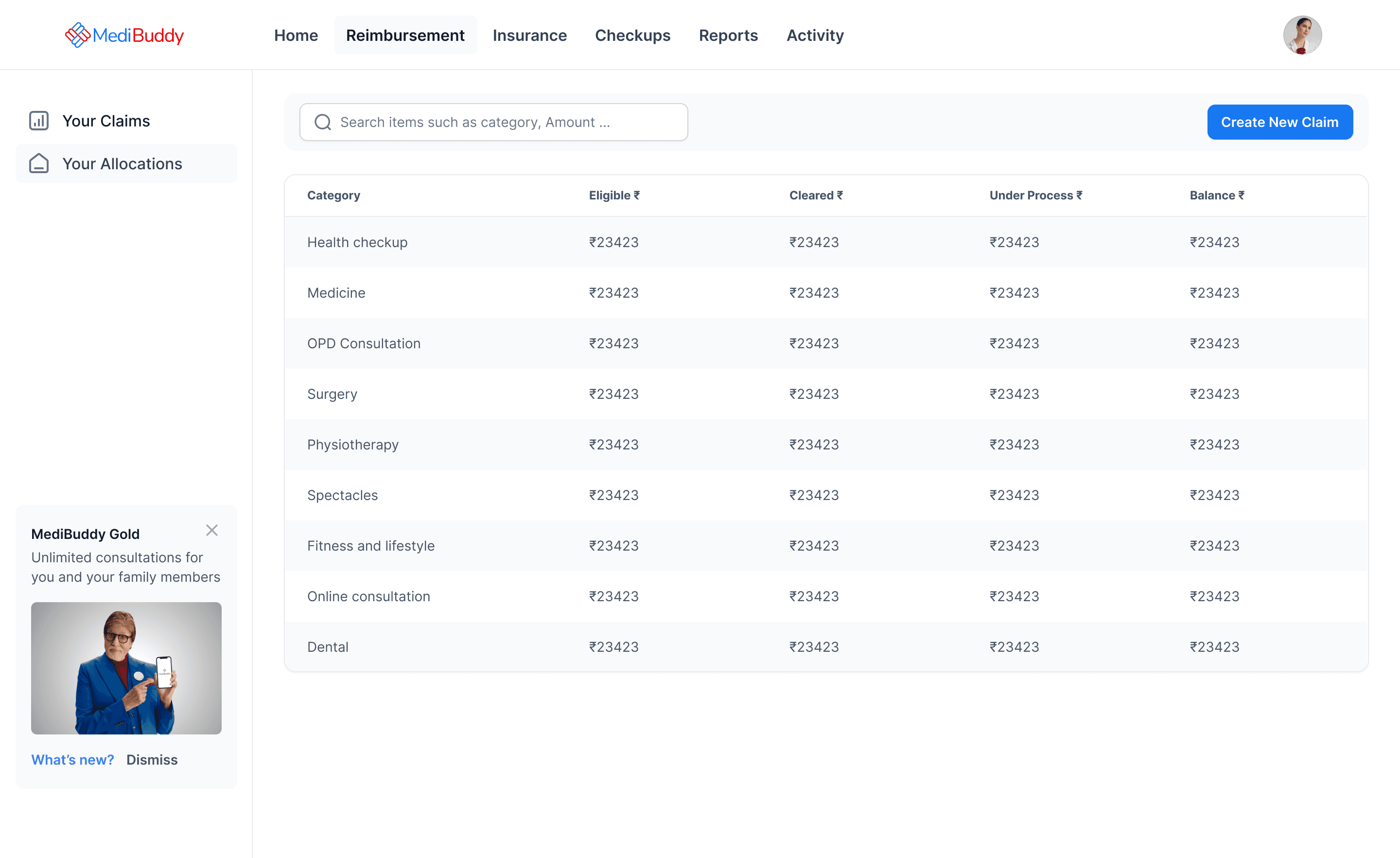
What is MediBuddy Reimbursement
MediBuddy Reimbursement is a feature that allows users to claim their medical expenses. Users must either be insured with an insurance provider partnered with MediBuddy or be part of a corporate health benefits program offered through MediBuddy. Eligible users can submit claims for medical bills across 12 different services, including consultations, lab tests, surgeries, medicines, physiotherapy, dental care, and more.
Problem Statement
• MediBuddy is not providing a platform where users can reimburse their medical bills, and it is a huge pain for users especially
corporate users.
• MediBuddy users are depending on TPA and other health services for claiming their bills where they have to go through many
physical steps as well as reaching out to the TPA office etc - User’s pain.
• MediBuddy doest know, For what all medical issues - the users are depending on other healthcare services for claiming.
• Depending on Medibuddy for all medical services such as online consultation, Lab tests, Medicine etc and Jumping on to the
other platform for Insurance is another pain of a user.
Secondary Research
The issues identified in the existing medical reimbursement system result in several significant negative impacts which are given below
Amidst of all the work, Running behind the Reimbursement process is indeed a hectic pain point of a corporate employee

Reaching out HRs and other finance team staffs are a hectic and head ache process
Hence the user cant see the process, Always getting anxious about the outcome
Breaking down user’s problems
Broke down user's problem so that the problem understanding can be much better and also was able to determine different aspects and verticals of the problems well
Complex
&
Delay in process
People
Dependancy
Process
not visible
Required
More effort
No voice
in between
Types of Medical services of MediBuddy
MediBuddy processes a wide range of medical services to facilitate seamless healthcare management for individuals and organizations. Our services encompass various types of claims, including hospitalisation claims, outpatient treatment claims, diagnostic tests claims, medication claims, and emergency medical claims.

About TPA - Medi Assist
Medi Assist provide third party administration services to insurance companies through our wholly owned subsidiaries, Medi Assist TPA, Medvantage TPA and Raksha TPA. Its Indian provider network comprises 18,000+ hospitals across 1,069 cities and towns and 31 states (including union territories) as on September 30, 2023. Medi Assist partners with group accounts (employers) to administer their employee health insurance plans, in India. Additionally, partner with Insurers to administer health insurance plans for retail customers (individual insurance Policyholders) and publicly funded health schemes (Government Schemes).
Issues of TPA
• Slow in process hence deals with 9000+ Corporate companies.
• Needs to go through physical process as well, like going to office of Mediassist to submit claim proofs etc.
• Users not satisfied with the claim amount which they get reimbursed.
• Overall service is not up to the mark.
Assumptions
• It would be beneficial for MediBuddy to include insurance claim options on the platform, alongside consultations, lab tests,
medications, dental services, and more.
• By understanding user requirements, MediBuddy can identify demand for additional medical claims, such as vision care.
• This approach would position MediBuddy as a comprehensive, one-stop platform for all medical services.
Why Now ?
Currently, we encourage our corporate users to access health services on MediBuddy through cashless wallets. However, some users still utilize external health services and seek reimbursement through their companies. Introducing a reimbursement option on MediBuddy would attract these users to our platform for filing claims. Additionally, it would provide insights into their reimbursement patterns and preferences, allowing us to transitio-n them from reimbursements to utilizing MediBuddy's cashless health services over time.
Research on internet
Conducted in-depth online research focused on insurance and medical bill claiming processes. Gathered valuable data on industry trends, user needs, and best practices to enhance our platform's features and user experience. Analyzed competitive solutions and identified key opportunities for improving Medibuddy's services.
User interview questions (To Users)
Process Understanding:
Can you describe your current process for submitting a medical reimbursement claim ?
What difficulties do you encounter when filling out the reimbursement forms ?
User Experience:
How intuitive do you find the current system for submitting claims?
What specific features or functionalities would make the submission process easier for you?
Feedback and Support:
How often do you need to contact customer support for help with your claims?
What kind of feedback or notifications would you like to receive during the claims process?
Timeliness:
How long does it usually take for your claim to be processed and reimbursed?
What delays have you experienced, and how do they affect you?
Suggestions for Improvement:
If you could change one thing about the current reimbursement system, what would it be?
How can the system better accommodate your needs and preferences?
User interview questions (To Verifiers)
Process Understanding:
Can you describe your current process for submitting a medical reimbursement claim ?
What difficulties do you encounter when filling out the reimbursement forms ?
User Experience:
How intuitive do you find the current system for submitting claims?
What specific features or functionalities would make the submission process easier for you?
Feedback and Support:
How often do you need to contact customer support for help with your claims?
What kind of feedback or notifications would you like to receive during the claims process?
Timeliness:
How long does it usually take for your claim to be processed and reimbursed?
What delays have you experienced, and how do they affect you?
Suggestions for Improvement:
If you could change one thing about the current reimbursement system, what would it be?
How can the system better accommodate your needs and preferences?
User requirements (Of User)
Process Understanding:
Description of Submission Process: "I usually have to gather all the necessary documents, fill out a detailed form, and submit it either online or by mail. It’s a bit cumbersome and takes a lot of time."
Difficulties Encountered: "The forms are confusing, and I’m never sure if I’m filling them out correctly. Sometimes, I miss required fields or documents, which causes delays."
User Experience:
Intuitiveness of the Current System: "The current system is not very user-friendly. It’s hard to navigate and understand what’s needed at each step."
Desired Features: "I would love to see a step-by-step guide or checklist that clearly outlines what I need to do. Auto-fill features for common fields would also be helpful."
Feedback and Support:
Frequency of Contacting Support: "I have to contact support almost every time I submit a claim, either to clarify requirements or to check the status of my claim."
Desired Feedback/Notifications: "I’d like to receive real-time updates on my claim status, including confirmation of receipt, processing stages, and final decision notifications."
Timeliness:
Claim Processing Time: "It usually takes a few weeks to a couple of months to get reimbursed. The waiting period is quite frustrating."
Experienced Delays: "I’ve had claims delayed due to missing documents or errors in my submission. These delays cause a lot of stress, especially when waiting for significant reimbursements."
Suggestions for Improvement:
One Change to the System: "I would make the form simpler and more intuitive. Clearer instructions and examples would be great."
Accommodating User Needs: "A user-friendly mobile app would be a game-changer. Also, better integration with healthcare providers to auto-fetch necessary documents would save a lot of time."
User requirements (Of Verifier)
Process Understanding:
Verification and Approval Process: "We receive the claims, check for completeness and accuracy, and verify the details against our records. It’s a multi-step process that involves several checks."
Common Errors/Issues: "The most common issues are incomplete forms, missing documents, and incorrect information. We often have to contact the claimant to correct these issues."
Efficiency and Bottlenecks:
Time-Consuming Steps: "Manual verification of documents and cross-checking information is very time-consuming. Sometimes we have to go back and forth with claimants multiple times."
Frequency of Returning Claims: "We return about 30-40% of claims to claimants for additional information or corrections, which significantly delays the process."
Tools and Support:
Current Tools/Systems: "We use a combination of an outdated software system and manual processes. The system isn’t very efficient and often requires manual data entry."
Effectiveness of Tools: "The current tools are not very effective. They lack automation and integration capabilities, which would make our work much easier."
Communication and Feedback:
Communication with Claimants: "We usually communicate via email or phone calls. It can be challenging to keep track of all the correspondence and ensure timely updates."
Desired Communication Improvements: "A centralized communication platform within the system would help. Automated notifications to claimants about the status of their claims would also be beneficial."
Suggestions for Improvement:
Desired Features/Changes: "We need better automation for document verification and data entry. A more intuitive interface for both claimants and approvers would also help streamline the process."
Supporting the Approval Process: "The system should include comprehensive error-checking features to reduce the number of incorrect submissions. Better integration with other healthcare systems would also be advantageous."
An assumption flow

Quantitative research
In quantitative research, i prepared a questionnaire in google form and shared with the corporate employees only went for claiming their bills. I received about 16 responses.

Competitor analysis
In conducting a comprehensive competitor analysis, I evaluated existing medical reimbursement systems currently available in the market. This analysis aimed to identify best practices, pinpoint areas for improvement, and gather insights that could inform the design and functionality of our system.
Apps in Market
Reimbursement
Insurance
Physical Document
Through HR
Visiting office
Claim Within 1 week
MediAssist
Vidhal
Reimbursify
Acko
Reimbursify
User Persona
Analysis and data collected from the interviews and surveys helped me to create personas which represented an ideal user of the application. The persona gave me insights to design a better solution. It helped me to understand the user goals, frustrations and the overall personality.
James Jacob
Age
28
Education
B.E Engineer
Status
Single
Occupation
Quality Engineer
Location
Bengaluru
Personality
Calm
Thinker
Creative
Breif Story
Mr. Amar Mahajan is a 28-year-oldIT professional from Bangalore, Works in database management at an IT company Spends workdays in the office; enjoys weekends with friends and family. Passionate about food and travel
Goals
• Easy reimbursement of medical bills
• Staying updated on claim processes
• Streamlining bill reimbursement with simpler procedures
Frustations
• Complex process of claiming medical bills
• Inability to claim bills independently
• Dependence on others for bill claiming
Motivations
• Getting bills claimed very fastly without anybody’s help
Interests
• Reading
• Music
• Movies
• Trekking
User journey map
The below user journey map shows a visual illustration of how the user is going to interact with the platform. The user journey map starts from the initial contact or discovery phase, and continues through the process of engagement till the extension phase. I have identified the key interactions and touch points that the user will come across while using the app. It has helped me to optimise the user experience of the reimbursement platform
Entice
Touchpoints
Enter
Engage
Exit
Extend
Hearing About reimbursement claiming platform from HR or colleges
Opening the Reimbursement module in HR Portal or in MediBuddy App
Home screen
Exposure to all main features such as creating a claim etc
Creating Claim
Uploading Personal details
Uploading Bank details
Uploading Bill Details
Terms and conditions
Submitting the bill
Successfully
Notification and confirmations
Closing the app and going through the notification or confirmatoin
Giving feedbacks about the services
Giving rating
Checking the status of the bill
Again using the reimbursement portal for claiming bills
Login
User flow
In this user flow I gave a visual representation for the user to map out each and every step the user takes from every point right through the final point. User flow is helpful for me to understand how a user navigates through the page and what decisions can they possibly make and complete app experience at a holistic level.

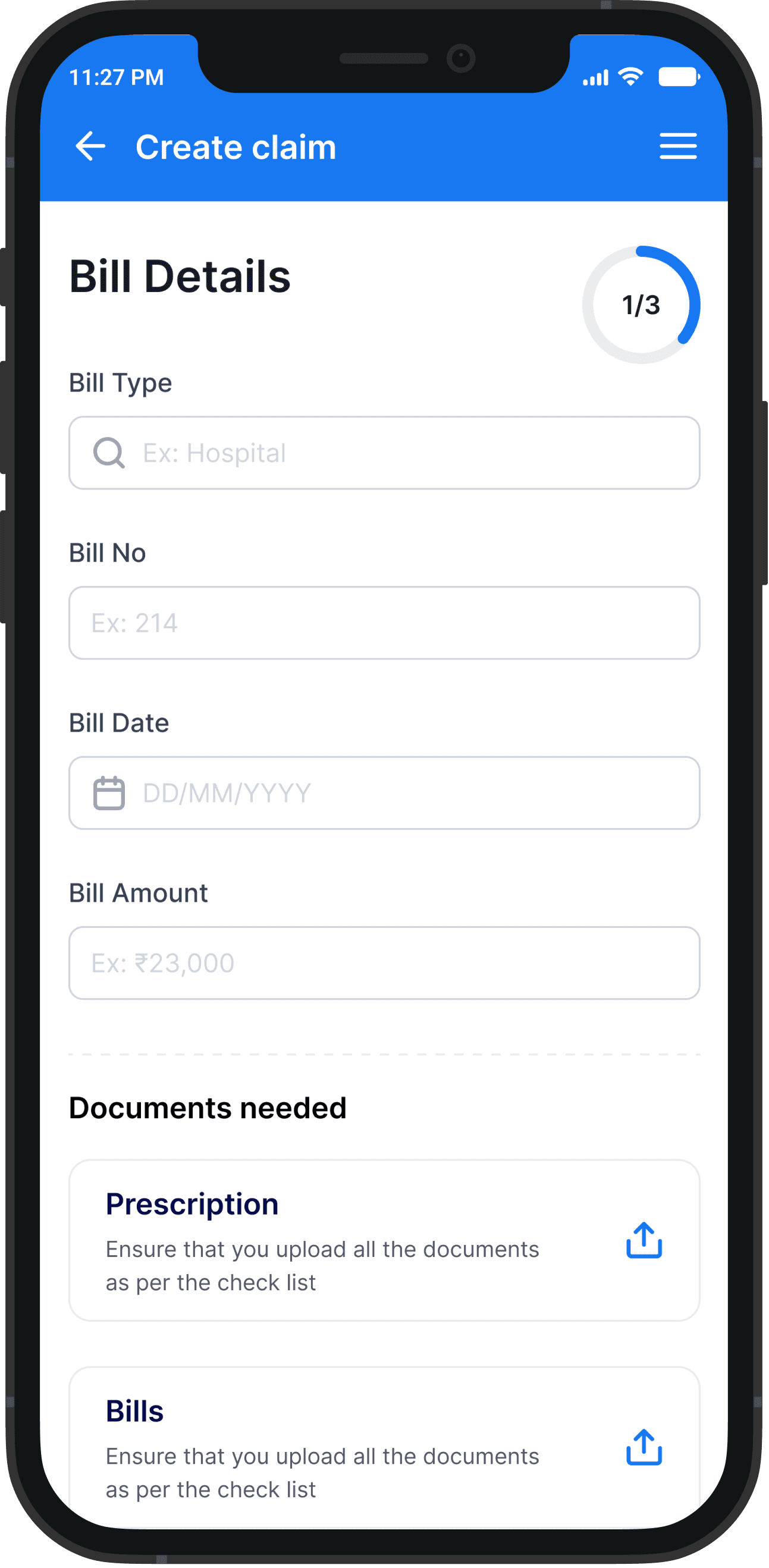
Few visual screens
An overview of the final product screens designed to streamline workflows








The Impact
Business Outcome
The medical reimbursement project for Wipro yielded significant business outcomes, aligning with our strategic objectives and delivering substantial value to our client.
60 M
Target achieved
Successfully met the target of INR 60 Million
3 k
User engagement
Attracted 3,000 Wipro employees to the platform.
12 k
Claim Processing
Processed 12,000 medical reimbursement claims.
20 k
Average Ticket Size
Managed an average reimbursement amount of 20,000 INR
per claim.
65%
Target achieved
Achieved a 65% reimbursement rate among users those who came to the platform
My learnings
Strong Collaboration with Developers Improves Execution
Close coordination with developers helped ensure that designs were technically feasible and accurately implemented. Early and continuous collaboration reduced rework and resulted in a more polished final product.
Continuous Stakeholder Alignment Strengthens the Product
Regular check-ins with stakeholders at every phase of the project ensured alignment on goals, constraints, and expectations. This ongoing communication helped catch issues early and led to better, more informed design decisions.
Involving Front-End Developers in UI Changes is Essential
Including front-end developers in any UI changes helped maintain design–development consistency and avoided
last-minute surprises. This collaboration ensured smoother handoffs and higher-quality outcomes.
Avoid Assumptions and Clarify Early
This project reinforced the importance of not designing based on assumptions. Asking questions and clarifying requirements early helped prevent misunderstandings, reduced rework, and ensured that design decisions were aligned with real user needs and business constraints.




